What’s inside:
Hospitals are looking to streamline supply chain workflows in Operating Rooms (OR) and Procedure Rooms.
Our CEO shares his thoughts on:
- The perioperative documentation challenges for nurses recording utilization in the EHR.
- The challenges of achieving full charge capture at the point of use.
- How new healthcare AI technology is addressing the surgical supply chain inefficiencies.
An opinion article by: Shlomo Matityaho, CEO of IDENTI Medical
We sat down with our Founder and CEO, Shlomo Matityaho, to talk about the issue of surgical supply documenation at the point of care. This is what he had to say.
Surgical spaces are the domain of nurses, so the burden of POU supply chain data collection falls upon their shoulders. It’s common, however, for longwinded workflows and inefficient tools to hinder their supply chain capabilities.
85% of nurses find supply chain workflows stressful, with a similar percentage highlighting documentation as a particular challenge.
20% of nurses are said to be considering leaving their job due to the frustration of dealing with supply chain issues.
Clunky systems and time-consuming workflows and manual workarounds are responsible for items being left unrecorded at the point of care. When the documentation of every item consumed in surgery is complicated and time consuming it frustrates nurses and risks data errors and omissions.
Poor tools to record surgical consumption can open the hospital up to risk:
- Patient safety risks: A survey found that 25% of nurse respondents didn’t have the time to check items for expiry and recall prior to consumption.
- Financial risks: Missed charge-capture at POU results in incomplete billing and under-reimbursement. Up to 52% of items are said to remain uncaptured after surgery. OR and Procedure Rooms are a known dollar drain in the supply chain.
Let’s look at why current workflows are failing.
Current POU item capture tools
Ensuring end-to-end tracking throughout the hospital supply chain is an important task. Healthcare providers use a range of systems to document usage at the point of care.
-
Manual workflow:
Some hospitals still use manual implant logs or the cutting-edge technology of stickers! To state the obvious, manual documentation fails to comply with FDA UDI regulations, which require the digital documentation of medical devices. Achieving a digital record will require the keying-in of item details into the EHR, ERP or other local system. This repetitive manual data-entry is time consuming and error prone.
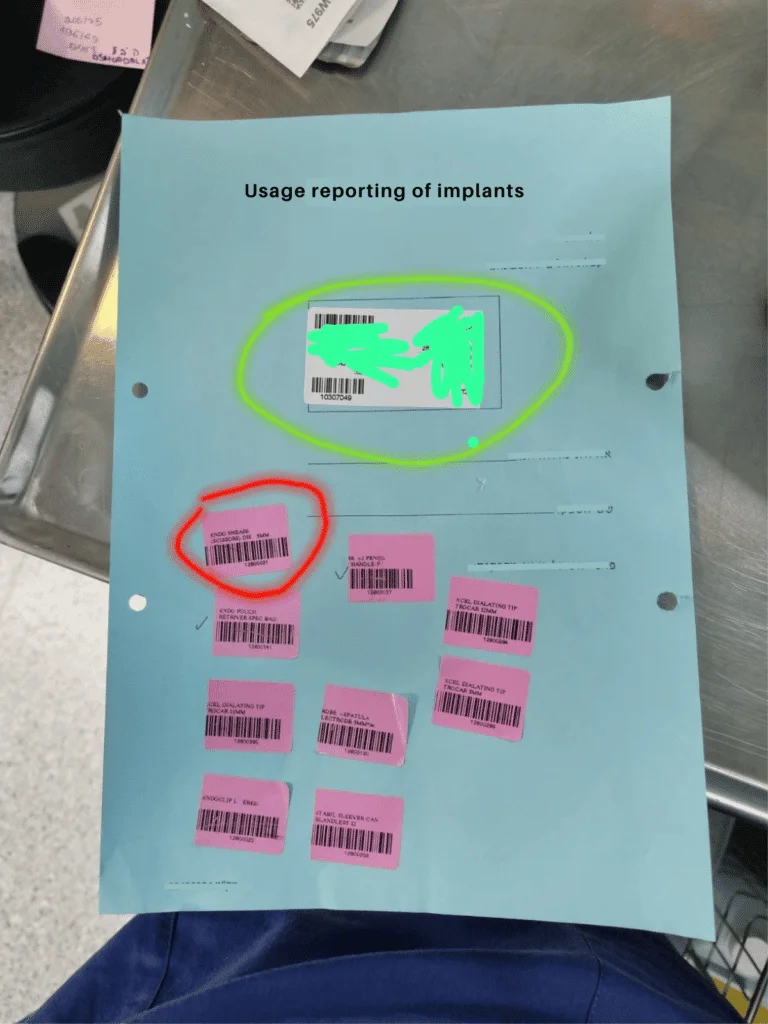
Reporting of implants using stickers and manual documentation in patient files
-
Traditional barcode technology:
Barcode or QR code scanners are commonly used to capture SKU data. Their main advantage is that they are cheap and readily available – but that’s where their main benefits end.
As any Circulating Nurse will tell you, they regularly fail to achieve the ultimate goal of capturing complete item information. Handheld scanning tools are presented as the easy answer, but there are many areas where they fall short.
There are three main reasons that barcode scanners fail to collect data on every item used in surgery:
-
-
Barcode UDI structure is constantly changing:
-
The UDI barcode (DI-PI) in the hospital Item Master require constant maintenance in order for barcode scanning to work. As teams rely upon the scanned item finding a match in the Master Catalog List, it has become a crucial barrier in the successful capture of charges.
-
-
Not on the Item Master:
-
Items such as trunk stock by-pass the materials management team and are delivered straight to the procedure room, without being recorded on hospital systems. Again, when the item is scanned… no Item Master match.
-
-
No barcode or multiple barcodes:
-
Orthopedic kits and trays are made up of individual and unlabeled items, with no barcode or tag, so that the item cannot be scanned. At the other end of the spectrum many products have a large number of barcodes, making it hard for nurses to identify the correct barcode to scan.
Barcode scanners often fail to fully record utilization in surgery. Frustrated Circulating Nurses are then faced with the painstaking task of keying-in all that missing data onto the hospital ERP.
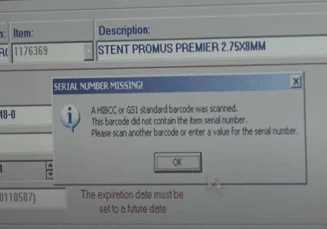
-
The complicated EHR and ERP software
The EHR/ERP updated by nurses during procedures provides source data for several other hospital systems. It’s therefore important that the POC data captured is comprehensive and correct.
When nurses need to add utilization data onto the ERP or EHR – whether it’s adding a new item that couldn’t be scanned or adding missing data to a scanned item – they have to endure longwinded workarounds.
The reality of adding data to an ERP system is that it involves trawling through numerous pages of a badly designed system, manually keying-in data into one field after another, and selecting items from a multitude of drop downs – it’s a laborious, error-prone process which needs to be carried out for every undocumented or partially documented item.
Nurses simply don’t have time for complicated admin, so more often than not, the item ends up unrecorded or with data gaps, resulting in no digital link being made between the product and the patient.
-
Computer Vision Technology:
A new, emerging, pain-free option for data capture is gaining momentum every day. Imagine an end to monotonous manual data entry and ineffective scanning and instead combining the speed and simplicity of a camera with smart software, that captures all the data you need.
Image-recognition technology is the new way that hospitals can achieve 100% itemization at the POU. This new approach is quick to use, doesn’t require RFID tags or barcodes, nor is it reliant upon the hospital’s Item Master List.
Having a visual record of usage captures full information, preventing data-gaps in the workflow. Think of yourself describing a route you travelled around Times Square NYC – wouldn’t be easier to show an image of your route instead of describing it?
Image capture makes the digital documentation of usage data a quick and simple task for busy nurses.

The benefits of an efficient POC item capture tool
Regardless the technology you choose, let’s look at the benefits of using the right POU tool to achieve 100% item and charge capture.
- Billing reconciliation: identifies lost revenues and improve reimbursement. Visibility to utilization can assist in transparency with vendors and negotiating contracts.
- Nurses can focus on nursing: When admin workflows are kept to a minimum, nurses can focus on patients, not solving logistic and charting issues. The knock-on effects are improved patient outcomes, increased nurse satisfaction and improved retention.
- A balanced inventory: When utilization is documented, end-to-end item tracking is achieved, resulting in full inventory visibility and accurate restocks.
- Patient safety: Timely usage documentation can provide pre-consumption expiry and recall alerts, plus robust post-procedure recall management – it literally saves lives. These steps ensure full regulatory compliance and provide enhanced patient protection.
- Value Based Healthcare: When reimbursement is dependent on patient health outcomes, there is direct financial reward for putting robust systems and procedures in place that boost patient safety.
- Full charge capture: Put simply, uncaptured charges are lost income. Digitally documenting full item charges ensures correct and timely cost of surgery billing, which results in optimal reimbursement.
The role of advanced data analytics in planning and performance
When full utilization data is collected, it has an impact long after the procedure has finished.
The best POU tools use inventory management software that provides real time metrics, reports and data insights. This crucial supply chain data gives managers up-to-date inventory visibility and historical trend data.
Data gives hospitals insight into their inventory, allowing them to identify areas of inefficiency and make evidence-based decisions.
Hospitals are finding that data is a key driver for reducing inventory, streamlining suppliers and making significant cost savings.
- One example of data supporting supply chain efficiency, is the use of ‘cost of surgery’ reports by individual physician. Physician pick-lists are often out of date and incomplete – they need careful review that takes account of supply chain considerations. These reports can steer difficult discussions with cold, hard facts, helping to achieve more cost-effective physician preference items (PPI), without impacting on patient outcomes.
- Reports are a key management tool for reducing variance and streamlining suppliers. They can also be used to gain control of expiry and recall management, reduce wastage and achieve a balanced inventory.
We can see now that if full usage data is not captured at the point of care, then there is a gaping hole in the information used by management. Incomplete data undermines the ability of hospitals to make smart supply chain decisions.
So, we are back to the importance of documenting the items used in surgery – the weak point in item tracking for most hospitals.
Nurses need simplicity when it comes to supply chain management
There is a massive knock-on effect to getting POC utilization right, so hospitals need to take action to help nurses succeed in their supply chain tasks.
Existing workflows and technology have failed – they simply cannot cope with the complexities of the OR and Procedure Room.
It’s time to understand that if we don’t give nurses simpler and more intuitive tools to operate, which are fully compatible with the existing workflow methods in operating rooms – it won’t work.
Find out about Snap&Go, a brand-new image recognition and AI technology for 100% item and charge capture at the point of care.
Contact us to find out how it could transform your surgical supply documentation.