What’s inside:
This article looks at medical device inventory management in healthcare facilities. It will cover:
- FDA UDI regulations on implant tracking
- Hospital inventory management challenges
- Healthcare inventory management processes
- RFID technology for managing medical devices and implants
- The link between inventory management and patient safety
- Technology to support robust recall management in healthcare
- HIPAA compliance
Medical device inventory management is a multi-billion-dollar market that is ever-changing as new products are developed and released.
Keeping track of the inventory for thousands of items from hundreds of manufacturers presents several issues, not including those faced by hospital administrators concerning costs and equipment maintenance.
Medical device inventory management is a challenge for many. The issue with tracking inventory is that with the use of barcodes on each item, there needs to be a large number of people involved to properly update information whenever an item changes hands.
There needs to be someone who scans the barcode when it is first received into stock, another person to scan it when it leaves their hand, and one more person before it can arrive at its final destination. Often this workflow gets so complicated since many people are involved, there are sometimes disconnects between who has what and whether or not the inventory counts add up. So, it’s a relief to hear that there is an automated solution to this problem, in the form of radio frequency (RFID) tags that can be used instead of barcodes.
Medical Device Tracking: FDA UDI Regulations
One important healthcare reality is that, in 2013 the US Food and Drug Administration (FDA) released a UDI rule which establishes a UDI system applying to all medical devices placed on the US market. These regulations were designed to add standardization and improved processes into medical device inventory management in healthcare. Following the FDA, the European Commission, and other regulators have made patient safety a strategic priority, by developing UDI regulations for implants and Medical Devices.
The UDI system was intended to provide easier traceability of surgical implants and medical devices, which significantly helps to reduce medical errors and to fight against falsified devices. Also, enhances the effectiveness of capturing safety and allows for better monitoring by competent authorities. The use of the UDI system finally should also improve purchasing and waste disposal policies and stock management by health institutions.
The regulation requires all medical devices and implants to include a unique device identifier (UDI) on device labels and packages and submit device information to the Global Unique Device Identification Database (GUDID), i.e. the US FDA UDI regulatory database.
All hospitals must use Automatic Identification and Data Capture (AIDC), which refers to the methods of automatically identifying objects, collecting data about them, and entering them directly into computer systems, without human involvement. Technologies typically considered as part of AIDC include QR codes, barcodes, RFID, biometrics, OCR, and the recent innovative technology: image recognition.
Medical device inventory management – data gaps
But, contrary to many expectations, reality reveals many gaps stemming from the use and utilization of technology in the field. Which in most cases did not stand the test of reality. This gap occurs at the clinical POC where electronic capture and documentation of UDI for implantable devices inpatient electronic health records (EHRs) is not routinely being done throughout the U.S. health care system. It is well-accepted that electronic documentation of UDI is a critical linchpin for broad availability of UDI and use in downstream activities surrounding medical devices.
Without the broad development of seamless, accurate, efficient systems to electronically capture and document UDI at the POC in hospital systems, the advancement of a realized UDI system faces a significant barrier.

Why is medical device inventory management so important in hospitals?
Medical Device inventory management is essential to ensuring that all medical professionals have the equipment they need for every patient. The success of a hospital’s medical team depends on this, as poor quality or missing equipment can put lives at risk. A person may be hesitant for any number of reasons to use substandard medical supplies; they might not believe these items will do their job properly, or it might even be due to superstition. If a person has doubts about the effectiveness of an item then there’s no way that their hesitance won’t affect how well they do their job.
Managing hospital inventory can also save hospitals money in terms of purchasing power and unnecessary replacement costs. Although some items require higher quantities than others, using too many results in using money that could be put to better use. If keeping track of inventory can help save even just a few dollars here and there, the overall impact is tremendous.
Hospitals cannot afford to have important equipment not available when it’s needed most; there is no room for error or waste when lives are on the line. Hospitals work tirelessly to make sure all supplies are accounted for, but how do they manage this with so many items? The answer lies with automated inventory tracking solutions.
Medical device inventory management processes
The process by which hospitals keep an accurate count of their inventory has gone unchanged for decades now, as traditional barcode scanning methods remain in use today. A complicated accounting system involving people entering data into spreadsheets was mainly used back then because electronic systems were not in place. This system involved a large number of people being involved with the process, and managing that many records by hand can be incredibly time-consuming and even costly in terms of expenses for ink and paper.
What hospitals do have to recognize is that inventory errors from barcode scanning tend to add up when so much data needs to be inputted manually. The problem is only made worse when there are equipment malfunctions or power outages, which results in manual corrections after the fact. While this system might work for small organizations where the turnover rate isn’t too high, it doesn’t hold up over time; whenever an item goes into storage or leaves a room then there’s always going to be room for mistakes to slip through.
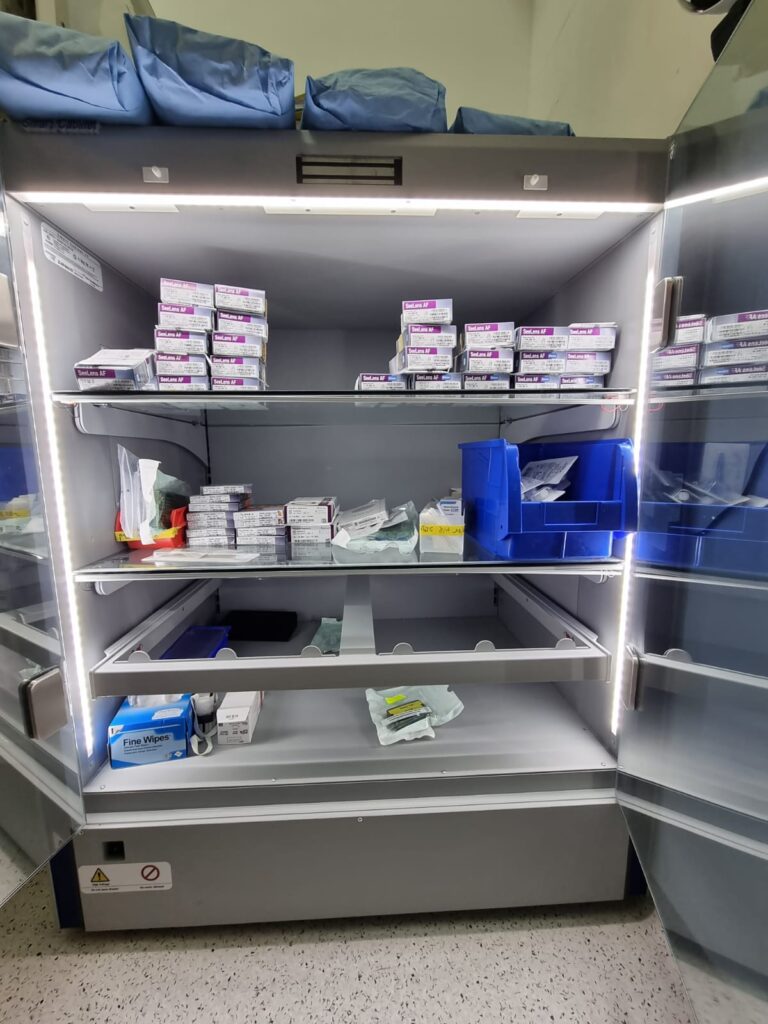
When an automated solution is implemented, using automated scanning via RFID tags, then data can be inputted automatically with very little room for error. Rather than having multiple people inputting data by hand, technology can handle all of this with ease, providing hospitals with accurate records in real-time. The great thing about this system is that it doesn’t matter where items are or who has them because they all have a tag attached to them. It’s the perfect way to keep track of inventory across a large network of medical personnel.
How does RFID work?
RFID are wireless devices that give off signals which machines are capable of picking up and interpreting on their own. They function by reading waves that come from the RFID tag when it’s in range, which is about a foot from the scanner.
RFID tags have been used in different applications for decades now, but it wasn’t until the early 2000s that they started to be used in hospitals and healthcare facilities. Studies found that even then there was still room for improvement; RFID healthcare technology itself works very well, but its implementation into this industry had room for drastic improvements.
Researchers discovered that largely due to hospital staff error and technical issues (including power outages), errors could end up compromising patient care. It was determined that with the current state of things many items would go unaccounted for or get lost entirely at some point; not only did this put equipment at risk of being nonoperational but it also put the people who work with that equipment at risk as well.
With these problems in mind, hospitals were encouraged to invest in modernized medical device inventory management systems which would be more reliable and accurate than what they had been doing before. This meant the implementation of RFID scanning technology rather than traditional barcode scanning methods used previously. With this change, there was an important shift from a manual process to an automated one which minimized human error.
By improving reliability and accuracy, hospitals can rest assured that their medical equipment is always going to be accessible when they need it most; this allows them to improve patient care while maximizing cost efficiency with regards to supplies for emergencies and day-to-day operations.

How patient safety is related to hospital inventory management?
Many hospitals make use of RFID technology in different ways to manage their inventory. For example, they can attach it to bed rails which keep patient beds in place, IV poles for fluid bags and tubing, wheelchairs and other transport equipment, cabinets containing medications, or even medical devices like splints or crutches. The great thing about this system is that it doesn’t matter where the items are or who has them at any given time because each one has its unique ID number.
When the hospital staff scans the tag on an item with a handheld device then their list automatically gets updated with current information; there’s no need to wait around for paper forms to be filled out manually so action can be right away. Through automation there are far fewer chances of human error being introduced, allowing hospitals to operate more efficiently.
Because each device has its ID number, the system is also capable of identifying exactly where an item is (and who it belongs to), what condition it’s in and how long it’s been since it was last checked. This kind of functionality allows for better tracking of equipment which reduces the risk that something might be missing or broken; this can prevent complications during surgeries or help them to save money on supplies.
Healthcare recall management
Hospitals are also required to perform a product recall which involves notifying patients of any potential dangers involved with using a specific piece of medical equipment. If the device has been damaged in some way or is missing then it might have had to be taken out of service until that’s resolved, which means that there are risks involved if they decide to use one instead of another for their treatments. However, because each device has its ID number hospitals can quickly find out what items are at risk and implement the necessary measures to prevent any accidents from happening.
The benefits for patient safety
Using RFID technology makes it possible for doctors and nurses to perform many actions on each item simultaneously. For example, if several pieces of medical equipment need to be cleaned at the same time they can just scan them all at once, eliminating the need for them to repeatedly take them out of service and back in each time they handle one. Also, because there are no forms that need to be filled out manually it brings down the risk of human error.
With RFID devices all completed tasks can also be tracked with ease since everything is stored on a computer system which brings up detailed reports but this means that there’s less chance of forgetting something or losing track of an item since it won’t get misplaced as easily compared to the old paper method. Being able to access patient records at any given time helps doctors and nurses provide better care because they’ll know exactly what was done before and what needs to be done next.

How does HIPAA compliance relate to hospital inventory management?
The Health Insurance Portability and Accountability Act of 1996 is a federal law that governs how patient information can be used. One of the requirements for this organization to comply with HIPAA is by ensuring that all forms have been filled out completely so there are no missing or improperly completed fields. Hospitals also need to keep records for at least six years after treatment because it’s required by state laws so if something happened during surgery they’ll have the necessary documents available, which makes it easier for them to defend themselves against any potential lawsuits. This means that hospitals cannot simply discard old forms they may still need.
When they started using RFID devices many of them found that their storage areas were becoming too small since they were now having to store more equipment. To compensate for this problem some of them opted to build additional storage areas or simply expand what was already there; either way, it’s adding extra expenses which they would rather not spend if possible.
One option that hospitals have is to bring in third-party vendors who can take old devices off their hands and make sure they’re disposed of properly before removing the tags so it becomes impossible to track where they are or find out any information about them at all. This satisfies HIPAA requirements because no one except the vendor will know exactly what happened with those items, making it nearly impossible for someone else to figure anything out.
Although using RFID devices has many benefits over the old paper method many hospitals still refuse to switch because it’s too expensive. Not only do they have to pay for the equipment one time and then continue paying for maintenance services but also need to invest in software that can handle patient records, which is an added expense.
Since many hospitals are facing budget cuts now more than ever it would be difficult to convince them that this technology is worth the cost, especially when there are other alternatives out there that are much cheaper but still effective.
When it comes to medical device management at medical facilities there doesn’t seem to be a standard way of doing things which makes it difficult for them because they don’t want employees spending unnecessary amounts of time looking for certain items or taking procedures out of service every time an item needs servicing or replacement parts need to be added or removed altogether. T
he idea of using RFID technology to track inventory may seem a bit unrealistic because it doesn’t have the necessary storage capacity but for those hospitals who have been struggling to meet HIPAA requirements and take inventory properly, this might be a viable option. The biggest question now is how many facilities will eventually decide to make the switch?
Find out about RFID inventory tracking solutions for medical device inventory management at your healthcare facility.
medical device inventory management
medical device inventory management
medical device inventory management
medical device inventory management






