What’s inside:
- Why operating room data collection is critical for hospital efficiency, compliance, and patient safety.
- How low compliance in reporting impacts costs, charge capture, and inventory management.
- The challenges of manual OR documentation and item master maintenance.
- How AI-powered OR supply chain automation improves accuracy, reduces errors, and streamlines operations.
Why is Operating Room Supply Chain Automation Critical for Hospital Efficiency?
The Hidden Cost of Incomplete OR Data
You’ve invested in technology, trained the medical staff, upgraded your EHR, updated the hospital SKUs, but still, the operating room’s usage reporting remains incomplete. Reports are inaccurate, charges are missing, and coding errors are frequent. Without effective operating room supply chain automation, these errors compound across clinical, financial, and compliance workflows. This affects compliance with FDA requirements, prevents accurate inventory tracking, and leads to significant financial losses; the very problems operating room supply chain automation solutions are designed to address.
Many hospitals attempt to deal with these challenges by purchasing supply chain management software. By 2026, the healthcare information industry is forecasted to grow by 8.2%. It seems that wherever we turn, we hear terms like Data Mining, Data Analysis, and Big Data.
Hospitals utilize advanced software solutions to improve processes, streamline workflow, and optimize resources. Yet while these solutions specialize in data management and analysis procurement processes, they are not tailored to real-time charge capture or operating room supply chain automation.
Any effective solution must answer the changing and exclusive needs of operating rooms, which differ greatly from other work areas.
For instance, the process of dispensing items is carried out in the OR by the medical staff, who do not specialize in supply management. In many ways, this process diverges from that of other logistics systems, in which the dispensing is done in a dedicated area, such as the cashier or in the warehouse, against a receipt or a delivery request.
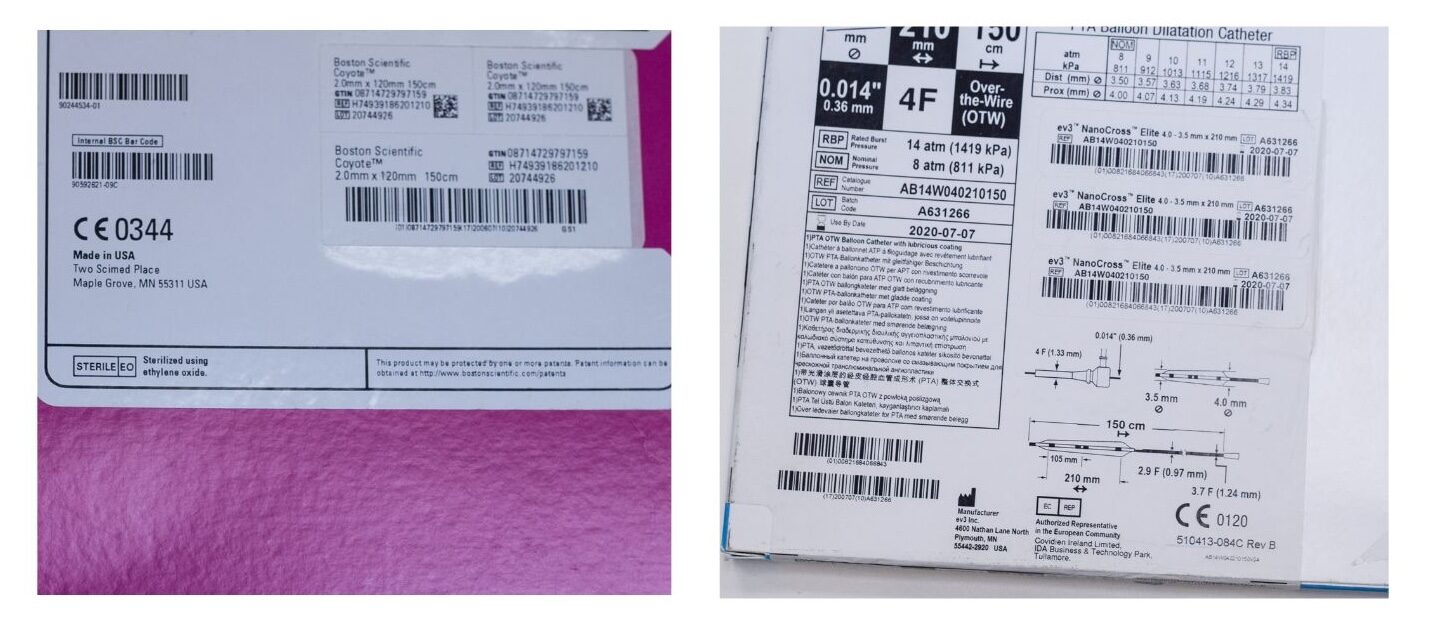
Another distinguishing factor of OR data collection stems from the structure and uniformity of the barcodes. While in other industries the structure and contents of the barcode are uniform, giving organizations the ability to rely on the barcodes received from suppliers, in the medical field, the reality is completely different. Hospitals cannot rely on the manufacturer’s bar code. It is necessary to attach an internal barcode sticker to the items, creating additional work for the OR staff registering the item into the hospital stock.
Add to this the fact that hospitals are increasingly moving toward a consignment model, which requires precise charge capture and a shared management system. These factors together raise a pressing need to create operating room supply chain automation software that works specifically inside the surgical environment.
Yet first, it is crucial to understand why collecting information in the OR is vital. How does it affect supply chain management and the hospital’s cash flow? From this understanding, clarified below, enhancing the collection of operational data as part of the medical procedure, with minimal reliance on the human factor in the OR, will come into focus.
The Financial Impact of Missing OR Data & How Automation Improves Charge Capture
Accurate Data Drives Revenue
Gathering information in the OR has enormous economic implications. First and foremost, it gives us the ability to know how much surgical procedures cost. Today, hospitals rely on historical DRG repositories, which in turn rely on statistical past analyses and general cost studies. Times have changed, technologies have changed, and AI operating room supply chain automation now makes real-time cost visibility possible.
An average hospital consumes about 5,000 implants and medical devices a month. Although hospitals strive to record each item individually, the level of reporting today is below 60%. In other words, the hospital has up-to-date information only on around half of the implants used. Why is the reporting level so low? Take items such as sewing thread or stampers: Though they are present in almost every procedure and can run up costs by $200 in some cases, they are not reported at all. In addition, items that cannot be tagged (such as sterile orthopedic implants – screws, plates, etc.), or bulk items are often not reported.
Add to this the time spent on coding errors and the need to submit applications for reimbursement from insurance companies or Medicare programs (which often require applications within 72 hours), and you have a full-fledged recipe for inefficient cost retrieval. Today, there is a whole market of companies that offer this service at a fee, and hospitals share with them the money received from the insurance company and government programs.
The Human Dimension: Why Automation Matters
Medical teams function under often stressful circumstances and focus on treating patients rather than on office work. This, alongside documentation that is carried out manually in notebooks or in complicated ERP programs, is a formula for error.
Research shows that procurement software and hospitals’ information management systems (ERPs) that are advanced and designed for health systems in practice slow down nurses’ work even more than manual documentation.
Indeed, human error, including coding errors and lack of reporting, is the main reason for the low compliance rate in the OR. Therefore, no matter how advanced the management software is, if it does not have the right tools to collect the information without involving the medical staff, it is not an appropriate solution that can achieve 100% reliability and integrity of data. This is why operating room supply chain automation focuses on removing manual steps entirely.
And for anyone who is wondering how there can be so many mistakes, the picture below shows two medical device packages. Which barcode would you scan?
The Cataloging Dimension: Maintaining an Accurate Item Master
The medical staff will rightly claim that even if it adheres to reporting usage of each item, and even if it receives training on logistics software, the software sometimes simply does not recognize the item in the operating room.
The first step in maintaining an updated item master begins with the consumption of the medical device. The medical staff needs to report the item, usually through scanning techniques. If the existing software does not identify the scanned item, the incomplete information needs to be completed from other sources.
Hospitals looking to maintain an accurate item master often face challenges in implementing operating room supply chain automation software that integrates manufacturer SKUs with internal hospital codes. This SKU does not specify an expiration date, production series, or other essential information about the item since that would require much work and the ability to read multiple manufacturers’ barcodes. The manufacturer’s SKU often changes, items age, and new suppliers are added, and as a result, the maintenance of the item master becomes one of the hospital’s biggest problems, with financial and clinical implications.
The Clinical Dimension: Patient Safety and Compliance
Generally, patients are oblivious to any logistical processes. We would probably never hear a patient before surgery asking a nurse to check the implant expiry date, even though it could be a life-threatening case. The patient relies on the hospital. The hospital relies on the medical staff.
Occasionally, there is a recall, which requires the hospitals and the supplier to locate all items and the patients who use the implants. This is an impossible task when there is no complete listing of all items used and full documentation in the patient’s medical file. A thorough process would be terribly time-consuming. Although the importance of the integrity of the information and the synchronization of the data is essential, unfortunately, the consolidation of such information is not the norm. Comprehensive operating room supply chain automation enables full traceability for recalls.
The Regulatory Dimension: MDR and FDA Compliance
Hospitals asking ‘How can we meet MDR requirements efficiently?’ can benefit from AI-enabled operating room supply chain automation that consolidates clinical and logistic data. When suspicion arises as to the safety of a product, medical organizations must provide critical information such as patient information, date, description of the case involving the medical device, brand information, product code, model number, serial number, expiration date, etc.
Yet in reality, without the consolidation of clinical and logistic information and high documentation compliance by the medical staff, hospitals are unable to provide the above information despite their obligation to do so. This is one of the main factors driving hospitals to purchase information management software.
Most of today’s tools rely on technologies that have been adapted to work in the operating room but do not fully address the problems mentioned here. In other words, advanced software does not include advanced data collection in the field. The full solution for consumption reporting and charge capture in the operating room has not yet been formulated.
Solution: The Digital Dimension
AI & Machine Learning: The Future of Operating Room Supply Chain Automation
Machine learning and AI-powered operating room supply chain automation allow hospitals to achieve full documentation, optimize inventory management, and accurately capture charges without burdening clinical staff.
In the digital dimension, the data is the goal rather than the means. The hospital must strive for 100% documentation in the OR – from medical devices and medications to a single sewing thread. Technologies that can autonomously collect data from the operating room exist in the world of machine learning.
Machine learning is a subset of computer science and artificial intelligence that refers to statistics and optimization. The main goal is to utilize real-world data to solve a particular problem when conventional software is insufficient. One of the capabilities is, for example, solving an identification problem that a human expert can solve, but is unable to produce specific software because the rules of identification change frequently, just like in the operating room.
Artificial intelligence is not uncommon, and we are already enjoying its services. In the near future, AI processing will be increasingly utilized in the field’s end devices, introducing new image processing technologies, OCR, ICR, microphones, or even sensors. These technologies can collect, process, and manage the information optimally.
The good news is that the future is in many ways already here. Hospitals are already investing money in comprehensive OR data collection solutions like Snap&Go to help complement their existing ERP systems. Software companies and ERP systems, for their part, are also investing money in developing such solutions. This trend is expected to intensify as more hospitals seek AI-powered OR supply chain automation to reduce errors and financial loss.