What’s inside:
This blog looks at the common problem of OR revenue leakage.
It’s the most difficult data-collection setting in the whole hospital, so how can providers optimize their OR revenue capture?
We discuss:
- The impact of OR data gaps
- How providers compensate for incomplete clinical usage data
- Common challenges faced by providers when documenting usage in OR
- How to fix point of use documentation issues
Operating rooms and procedural spaces are the highest revenue generator for healthcare organizations, so why is it that the systems and tools used to capture charges are so ill-suited to the job?
The impact of data leakage in OR
Good RCM is dependent on accurate and timely data – but achieving this is far from simple in the complex surgical environment. When there’s low data integrity in OR and procedural rooms, it has consequences across the organization.
This vital data drives internal processes by feeding admin and operational workflows, so it is inaccurate and incomplete it will result in:
- Additional admin hours to reconcile records and correct/update the system.
- Inefficient charge capture and compromised revenue.
- Inaccurate procurement due to imprecise usage data
- Raised patient risk due to incomplete patient records that can’t be relied upon in the event of a product recall or medical complication.
- Flawed management decisions based on partial vision.
Simply put – bad data in OR impacts on organizational operations and management.
Compensating for incomplete clinical usage data
Collecting utilization data from OR and procedure rooms is a common problem for healthcare providers.
In fact, it’s such an ongoing issue that providers often build a safety net into their processes, to compensate for known OR data deficiencies.
Common ‘coping mechanisms’ include:
- An additional nurse brought in to focus just on surgical documentation.
- Post-surgery documentation activity by the circulating nurse (that likely requires backfill to keep up with the OR schedule).
- Internal documentation reviews and reconciliations by cross-functional staff.
There’s a high cost to all of these activities, but healthcare providers can recoup some income that would otherwise have been lost. However, it’s a bit like shutting the stable door AFTER the horse has bolted. There’s no getting past the fact that it’s a resource-heavy, reactive approach.
Wouldn’t it be far more efficient to be proactive and collect full product and charge capture before the end of surgery? To close the door BEFORE the horse bolts?
What if all that time-consuming compensatory activity was no longer needed?
The truth is that new technology is transforming surgical documentation and charge capture – ensuring every reportable and billable item makes it into the system.
Common challenges documenting usage in OR
The top five challenges that customers face in capturing and recording surgical usage data are:
| OR Data Capture Challenge | Details on why this challenge risks non documentation at the point of care |
| Reliance on barcodes | Barcode scanning has known limitations in terms of capturing all the required information without additional keying-in. In addition, smaller items such as nuts, bolts and screws don’t have barcodes on them. |
| Reliance on manual data entry | Manual entry may be the only method used, or the fallback method when barcode scanning, or other systems fail to record all items or full data. Systems are slow and clunky, and errors and omissions are common. |
| Reliance on the Item Master | Products need to be identified before they can be entered into the system. The Item Master struggles to remain up to date with new products and code changes. Bill-only items also present an issue when they are not preloaded into the system. Lack of Item Master pairing prevents routine usage documentation. |
| Reliance on nurses | Perioperative nurses in OR need to focus on the patient and support the clinical team. Longwinded product usage documentation during surgery cannot be their priority. |
| Reliance on siloed systems | Some nurses need to make duplicate entries into two or more systems – each entry risks errors and omissions. Lack of integration between systems impacts directly on the integrity of data. |
If preventing revenue loss in surgical areas is important to you, then it’s time to investigate the pivotal role that new technology can play in reversing OR data leakage.
It’s time to achieve accurate consumption data before the patient’s been wheeled out of surgery!
Fixing point of use documentation issues
It’s clear that old technology and manual methods have failed to cope with the complexity of item tracking and charge capture in surgical areas.
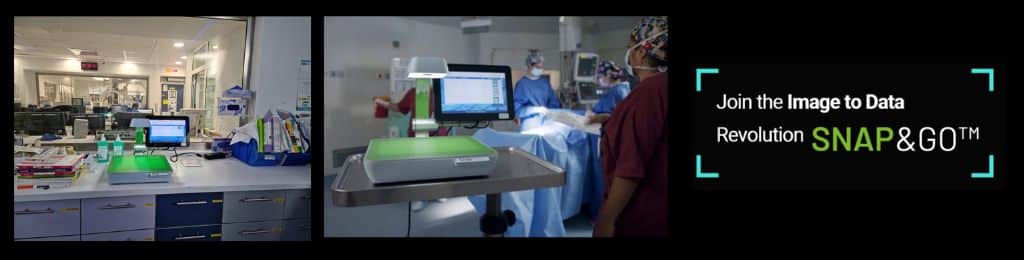
Image recognition and AI technology provide a different approach to item capture, product identification and system documentation.
Finally, nurses can be free from scanning difficulties, system errors, and mundane manual data entry.
New point-of-use documentation systems using image recognition technology are quick and easy for nurses, who just need to place each item under the sensor. A digital image is recorded in seconds, and the system then interprets and records all data on the package – including full UDI, batch number, expiry date and more.
Once nurses have completed this simple method of item capture, no further action is required by them, as the rest of the process is fully automated.
Item identification no longer needs to rely on the hospital having an up-to-date Item Master, instead sophisticated systems can tap into a global SKU database, where pooled data is constantly updated, making item matching a simple task.
And finally, seamless integration with hospital systems makes sure that real-time data is fed through to the EHR, ERP and MMIS for full documentation that feeds internal workflows in a timely manner.
New technology to collect and record clinical usage is plugging data leaks, and the impact is huge – optimized OR revenue, enhanced patient safety, streamlined workflows and improved operational efficiency.
Contact us to discuss how adding an image recognition sensor to your OR will support optimized OR performance.






