What’s inside:
Learn how limited supply visibility affects hospital financial performance at an enterprise level, specifically how it contributes to margin volatility, revenue leakage, cash constraints, and weaker financial governance.
It also explains why traditional, manual inventory approaches fail to address these issues and why some hospitals are reframing supply visibility as a financial control capability rather than just an operational function.
Why Hospital Financial Performance Suffers Without Real-Time Supply Visibility
In many hospital systems, finance leaders have a precise understanding of where margin pressure should be coming from, yet far less certainty about where it actually is.
They can explain labor productivity trends. They can model reimbursement changes. They can forecast payer mix scenarios with confidence. But when supply expense rises unexpectedly, or revenue underperforms despite stable volumes, the explanation often comes later, after reconciliation, variance analysis, and manual review.
That delay is not incidental. It is a structural weakness, and it shows up directly in hospital financial performance. The problem is not that hospitals lack data. It is that supply usage at the point of care, one of the most consequential drivers of cost and revenue, remains largely invisible in real time, even as care is delivered.
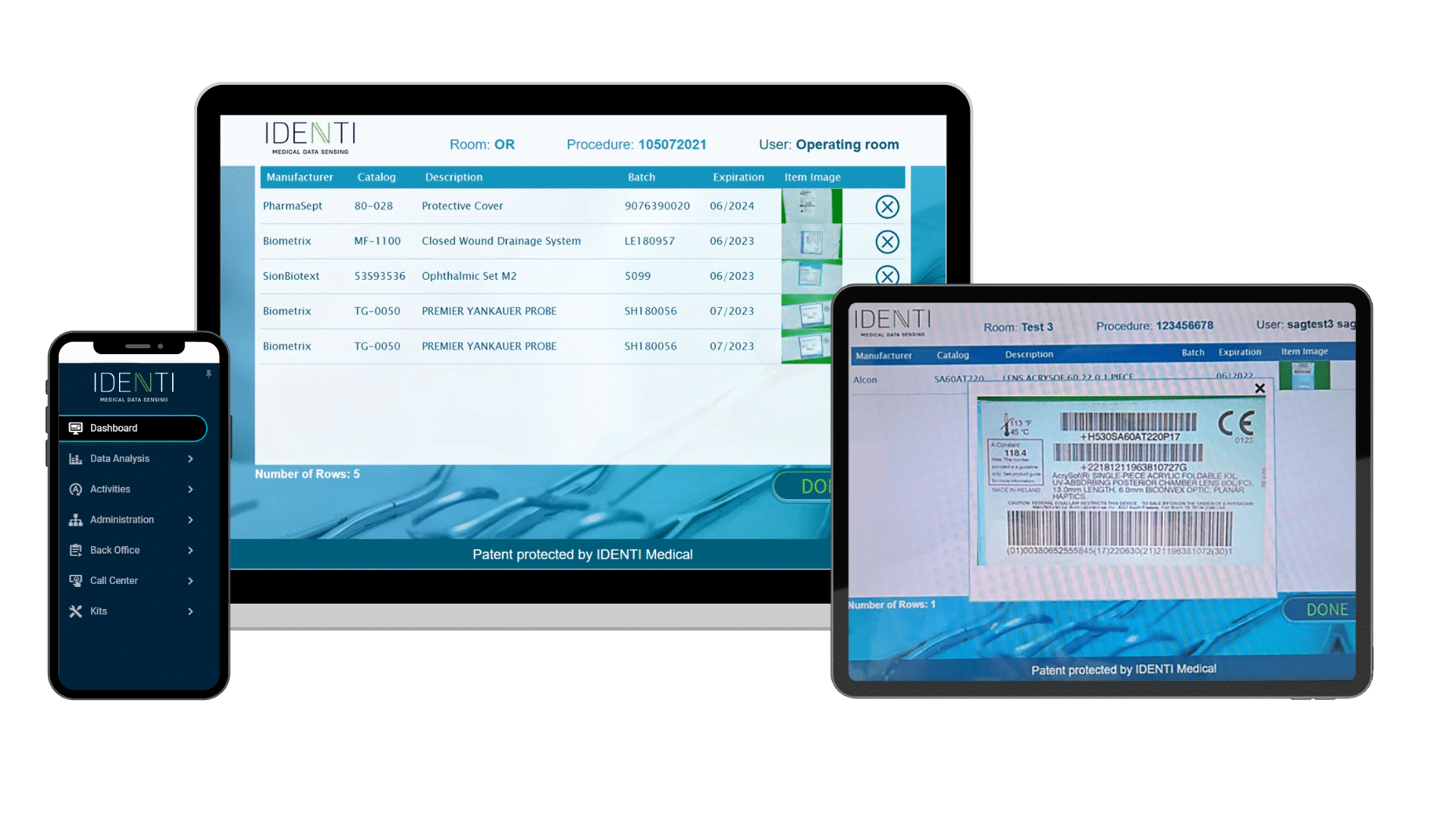
Real-time visibility only becomes possible when supply usage is captured automatically at the point of care, rather than reconstructed later through manual workflows.
What Are the Primary Drivers of Hospital Financial Performance?
To understand the impact of supply visibility, we must look at the four interconnected forces that shape a hospital’s fiscal health:
Hospital financial performance is shaped by four tightly connected drivers: cost control, revenue integrity, cash flow and liquidity, and financial governance. Together, they determine not only margin, but also predictability and control. When even one of these drivers operates outside real-time visibility, financial performance becomes harder to manage and easier to explain only after the fact.
Most leadership attention flows to labor and reimbursement because those drivers are visible, measurable, and familiar. By contrast, supply usage is fundamentally different. It is decentralized across clinical workflows, highly variable by case and provider, and influenced by day-to-day clinical decisions.
With manual tracking, supply usage operates outside real-time financial visibility, and it often escapes proactive management. Manual tracking incurs delays, while automated capture at the point of use alters the timing of financial insight, which is what makes real-time financial control possible. Meaning by the time its impact is visible in financial reports, the opportunity to intervene has passed.
Financial performance ultimately depends on what leaders can see in time to act. When major cost and revenue drivers sit outside that window, performance management becomes retrospective by default.
Margin Stability is a Visibility Problem, Not Just a Cost Problem
Hospital financial performance is an outcome, but control is the mechanism that produces it. Most hospitals rely heavily on lagging indicators: month-end closes, retrospective variance explanations, and post-period reconciliation. While this works for fixed costs, it fails for supply usage, which is usually dynamic and generated continuously at the point of care.
The Risk of Managing by History
When financial insight arrives weeks after a clinical event, leaders are forced to manage based on history rather than current conditions. This disconnect undermines margin stability by limiting the ability to course-correct before a budget variance becomes a permanent loss.
Without automated capture, real-time visibility remains aspirational rather than operational.
Supply Expense Is a Variable Cost That Few Hospitals Truly Control
For most health systems, supply expense represents the second-largest line item after labor. Yet, governance of this spend is often indirect. Traditional inventory systems are designed for availability (is the product on the shelf?) rather than accountability (why is the cost changing?).
Without real-time data, cost variation becomes normalized, and forecast confidence erodes. Hospital financial performance suffers not from a lack of discipline, but from a lack of timely, actionable insight into high-value clinical consumption.
How Real-Time Supply Visibility Protects Revenue Integrity
Financial performance is not only about controlling costs; it is about protecting earned revenue. Revenue leakage begins exactly where supply usage visibility ends.
Preventing Missed Charges at the Point of Care
Supplies used but not captured accurately at the point of care fail to convert into billable events. Documentation delays and manual handoffs introduce gaps that downstream revenue cycle teams struggle to close.
The financial consequences are predictable. Net patient revenue is understated when supplies used at the point of care are not captured accurately. Revenue integrity teams absorb growing rework as they attempt to reconcile usage after the fact, often across disconnected systems. Write-offs persist when documentation arrives too late to support a defensible claim. Over time, these losses compound quietly, eroding hospital financial performance without triggering immediate alarms.
Optimizing Working Capital and Hospital Cash Flow
Inventory is an operational asset, but financially, it represents immobilized working capital. When leaders lack confidence in real-time usage data, they compensate by increasing safety stock and PAR levels.
This “defensive” accumulation of inventory traps cash that could otherwise be used for strategic investments or debt reduction. Poor visibility constrains liquidity, increasing carrying costs and reducing the organization’s overall financial flexibility.
Strengthening Financial Metrics with Real-Time Data
For hospital financial performance to be credible, not just precise, leaders must trust that financial metrics reflect what actually occurred at the point of care. When supply data is inferred or averaged, forecasts become unreliable. Real-time visibility strengthens hospital financial performance by aligning financial reporting with “operational truth.”
By understanding exactly what was consumed, rather than what was reconstructed after the fact, CFOs can provide more accurate case costing and margin reviews to the board.
From Inventory Management to Financial Control: A Strategic Shift
Many hospitals confuse “inventory awareness” (knowing what is in the stockroom) with “financial control” (knowing the financial impact of usage in real-time).
AI and automation in healthcare finance depend on high-fidelity, timely inputs. This shift requires moving from manual documentation to automated capture of supply usage as it occurs. Without real-time usage data, even the most advanced predictive tools operate on approximations. Real-time visibility converts clinical activity into financial intelligence, allowing leaders to:
- Address cost drift mid-period.
- Prevent revenue leakage at the source.
- Base inventory decisions on actual demand rather than “just-in-case” hoarding.
Building a Resilient Financial Foundation
Hospital financial performance suffers when leaders are forced to lead while looking in the rearview mirror. While real-time supply visibility doesn’t eliminate financial pressure, it restores the control necessary to manage it. Hospitals that capture supply usage as it happens are building a more resilient, predictable, and financially defensible foundation for the future of care.






