What’s inside:
- What CMS’s TEAM model includes, and which procedures fall under its bundled payment structure
- The new reporting and reconciliation rules hospitals will face under TEAM
- Why documentation accuracy directly impacts audit readiness, risk adjustment, and revenue
- Common documentation blind spots that may lead to reconciliation losses
- Steps hospitals can take now to align data capture, finance, and compliance processes
- How IDENTI’s automated documentation platform supports TEAM readiness and real-time cost validation
As hospitals prepare for CMS’s Transforming Episode Accountability Model (TEAM), the coming shift in reimbursement will test a foundational capability: a hospital’s ability to document precisely, completely, and in real time.
Documentation isn’t just about recordkeeping, and in a value-based reimbursement era, automation is no longer optional — it’s the foundation for financial accuracy and compliance
What is CMS’s TEAM?
TEAM is CMS’s next-generation value-based reimbursement model, building on previous models, to expand bundled payments and improve care coordination. TEAM will cover five major surgical episodes, including joint replacement, spinal fusion, and select cardiac procedures. Starting January 1, 2026, it will require mandatory participation for selected hospitals in designated core-based statistical areas (CBSAs).
Under TEAM, hospitals will continue billing Medicare through traditional fee-for-service claims, but CMS will retrospectively reconcile total episode costs against a pre-set target price, effectively turning fee-for-service data into a bundled payment model.
Hospitals that deliver care below the target and meet quality benchmarks can retain shared savings, while those in downside-risk tracks may be required to repay CMS if costs exceed the target after Year 1.
The model’s goal is simple but it’s impact on hospital finance is significant. It’s designed to align financial incentives across providers, tie payment to quality and efficiency, and hold hospitals accountable for the total cost of care throughout the surgical episode and 30 days post-discharge.
On paper, that looks like a cost-control challenge. In practice, it’s a documentation challenge.
Why Documentation Is the Hidden Driver of Reimbursement
TEAM isn’t just a test of cost control — it’s a test of visibility. Every implant, supply, service, and post-acute intervention adds to the total cost of a surgical episode. If usage isn’t properly captured, hospitals face three critical risks:
- Reimbursement loss: Missed or delayed documentation can shrink shared savings or trigger audit findings.
- Target price overruns: Missed or delayed documentation can shrink shared savings or trigger audit findings.
- Weaker risk adjustment: Gaps in patient data can lower target prices, even when caring for more complex patients.
Consider two hospitals performing the same joint replacement. Both deliver excellent outcomes, but only one captures every implant and supply in real time. That hospital can validate its episode costs, demonstrate efficiency, and secure shared savings. The other faces reconciliation losses. Under TEAM, data tells your hospital’s story — and incomplete data tells the wrong one.
Even hospitals that thrive under fee-for-service often struggle to track product use and to link clinical and supply chain data in real time. Under TEAM, those gaps directly affect cost reporting, target pricing, and quality performance. Without accurate hospital documentation, hospitals may not be able to defend their costs or their outcomes.
Documentation as a Strategic Imperative
Documentation has long been treated as an administrative task. Under TEAM, it becomes a strategic asset — one that directly impacts revenue, audit readiness, and hospital margins.
Hospitals that treat documentation as a strategic capability will be positioned to:
- Reconcile usage and costs in real time
- Secure fair reimbursement by ensuring risk adjustment reflects true patient complexity
- Demonstrate efficiency and quality in value-based reimbursement models
This is where alignment matters. Clinical teams must capture product use in real time, supply chain leaders must ensure cost data is accurate, and finance must reconcile usage with claims. Documentation for value-based reimbursement models isn’t siloed in one department but is enterprise-wide, especially when TEAM covers an entire episode of care and requires provider collaboration, continuity of care, and focus on positive long-term outcomes.
How IDENTI Empowers Hospitals to Succeed Under TEAM
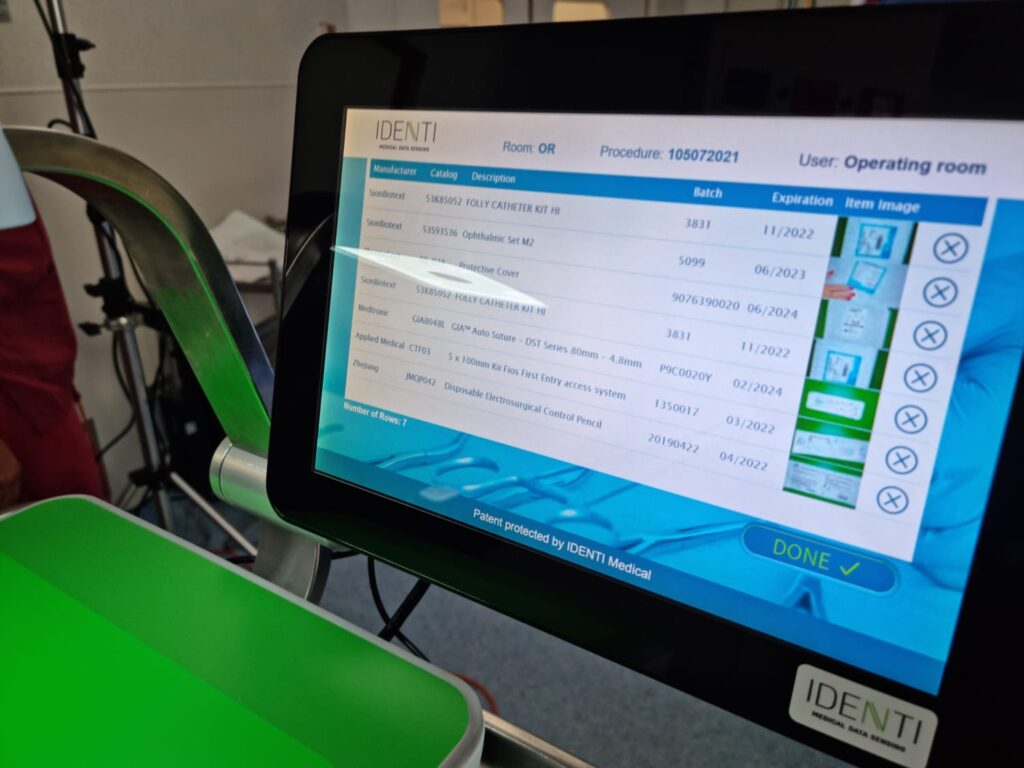
IDENTI’s digital platform eliminates documentation blind spots by automatically capturing every implant, device, and supply at the point of care and linking it directly to the patient, physician, and procedure. With clean, automated data, hospitals can:
- Reconcile usage and costs instantly
- Strengthen audit readiness and defend reimbursement
- Enable analytics that reveal cost and utilization trends
- Align supply chain, finance, and clinical teams on one unified dataset
With tools like Snap&Go, capturing all products used at the point of care, hospitals can feel confident about tracking their true spending costs and smartly stay under CMS’s target price.
Preparing for the Future of Value-Based Reimbursement in Healthcare
TEAM’s launch marks a turning point in how hospitals approach reimbursement. Those that invest now in real-time documentation and analytics will enter 2026 ready to manage costs, prove value, and protect margins.
For hospital leaders, the strategy is clear:
- Treat documentation as a financial function, not an administrative one
- Break down silos between clinical, supply chain, and finance data
- Leverage automation to ensure every charge, implant, and supply is captured accurately
- Ensure care pathways, provider alignment, and audit readiness accompany documentation accuracy
In value-based reimbursement models, precision = performance, and under TEAM, documentation can make or break a hospital’s financial success.
For healthcare leaders navigating this transformation, one truth stands out: to succeed under TEAM, you must start by treating documentation as a core business strategy.
Contact us today to learn how your hospital can prepare for TEAM and maximize value-based reimbursement.