What’s inside:
Watch our interview with IDENTI’s Lisa Miller to learn how your hospital can prepare for TEAM.
- Prepare for the CMS TEAM payment model
- Use automatic charge capture to accurately track product usage
- Identify opportunities to reduce cost variation
- Strengthen compliance and performance under TEAM
The Transforming Episode Accountability Model (TEAM) is redefining how hospitals manage costs, quality, and accountability for patient outcomes. Beginning January 1, 2026, the Centers for Medicare & Medicaid Services (CMS) will launch TEAM, a mandatory bundled payment program that holds hospitals responsible for both the cost and quality of care for 30 days after specific inpatient procedures.
Under the CMS TEAM payment model, hospitals must coordinate care across an entire episode, from surgery through post-acute recovery, while meeting cost and quality benchmarks.
In this interview, Lisa Miller, Chief Sales Officer at IDENTI Medical, explains the challenges and opportunities that come with TEAM. She highlights how understanding true surgical case costs and improving care team collaboration are essential for success.
Lisa also details how IDENTI Medical’s patent-protected Snap&Go™ computer vision ensures hospitals can gain complete visibility into every implant and supply used in surgery. Using computer vision and machine learning, Snap&Go™ automatically captures 100% of product and implant data in real time, giving hospitals accurate documentation and actionable insights into their true costs per procedure. This AI-driven charge capture not only enhances revenue integrity but also ensures hospitals have the precise data they need to meet TEAM’s cost and quality targets.
Watch the full interview to learn how your hospital can prepare for the CMS TEAM payment model, use automatic charge capture to accurately track product usage to understand real costs, and succeed under TEAM.
Want to learn how Snap&Go can prepare your hospital for the CMS TEAM payment model?
Understanding the CMS TEAM Payment Model: A Conversation With Lisa Miller
Natalie Foster (NF): Today, I’m speaking with Lisa Miller, IDENTI Medical’s chief sales officer. Lisa has extensive experience in hospital operations, specifically focusing on surgical services, patient experience, and overall hospital performance improvement. Today, we’ll be discussing the Transforming Episode Accountability Model, or TEAM, a new payment model from the Centers for Medicare and Medicaid Services set to roll out to hospitals across the US on January 1st, 2026. So we’ll break down what TEAM is, what hospitals need to know, and how AI-powered automation solutions can help them succeed under this new model.
What Is the CMS TEAM Payment Model?
NF: Lisa, thanks for joining me. Let’s start really at the beginning. What is the CMS TEAM payment model, and what do hospitals need to know about this new structure?
Lisa Miller (LM): Great. Thank you, Natalie, for having me today. I’m super excited about having this discussion with you, particularly because I feel IDENTI Medical can address some of the aspects of TEAM really well, and we can talk about it later and support hospitals in this new bundled payment. So first things first, I think now hospitals are getting their arms around the CMS TEAM Payment Model. When it was initially rolled out, I think everyone was unsure, but as I’m seeing and talking to hospitals, they’re having more meetings, they’re planning because really, it’s about two months away. So to answer your question, in this bundled payment model, a hospital is responsible for the care and the cost for thirty days for specific DRGs. So I’ll go in-depth about what those costs are, but we’ll start with the episodes.
The episodes included in the CMS TEAM payment model are:
- CABG procedures
- lower extremity joint replacement,
- major bowel procedure
- spinal fusions
- surgical hip/femur fracture
They DRGs represent that highest Medicare volume and cost. So it’s specifically targeted, I believe, from CMS because those are high volume, high cost, and as we have an aging population, they will increase as well. So they’re going to become higher cost and larger volume. I do think it was very timely because of our population. I also think that Medicare will increase the number of DRGs and add to that. But they started here. If you go back, hospitals are familiar with CJR and BPCI, so bundled payments and also total knee, total hip joint replacements that happened previously. So based on a lot of that learning, they’ve now come out with TEAM.
TEAM covers cost for a hospital, inpatient services, physician services, all the things that happen in the hospital, as well as post-surgery. So, 30 days post-op, which a lot of people feel, which is true just based on other bundled payments, that’s where a lot of the costs lie. Right? Where do the patients go? Do they go to a skilled nursing facility (SNF)? Are they going home with rehab? And also a big aspect is readmissions. So, the patient goes home, and something’s gone wrong, and now they go back to the ER and readmissions. And of course, the hospital’s got to manage all of that, including the readmissions. So that’s the 30,000-foot view. There’s a lot, too. I think there are 490 pages in CMS talking about TEAM. That’s the high level.
The Biggest Challenge for Hospitals Under TEAM
NF: And from your perspective, then, what is the single biggest challenge you think hospitals will face under TEAM?
LM: That’s an interesting question because I think there are a number of challenges. I think I’ll land on one. I think I might also let them have a secondary. I think one is really understanding the true costs of the case of those episodes from end to end, everything, what are the costs. From what I’m understanding and hearing, that’s what the hospitals are trying to get their understanding of—maybe they can get to what the surgery costs are. I still think that’s a problem. I think that’s where IDENTI can really help significantly. They’re really struggling with, okay, what does that post-surgery cost look like to manage the patient post-op?
I think secondarily, it’s just getting everybody organized. The collaboration, where they’re going to put care navigators, there are a lot of new aspects to the ruling where CMS is requiring a primary care physician pre-surgery. So that person, that doctor, has to be identified pre-surgery, and then that post-op, that schedule for that appointment has to be made in a certain number of days. There are also some additional questions and quality metrics, so it’s cost and quality metrics are added to this. How do you collaborate amongst all of those care providers and amongst five DRGs? I think there are two aspects—I landed on two.
How CMS Sets Target Prices Under TEAM
NF: Absolutely. Yeah, it really is breaking down silos between different departments and different systems and really causing people to look at what’s happening and the big picture. And so CMS sets a target price. So we started to talk about the cost a little. So each episode is given a specific target cost by CMS and based on some previous Medicare Part A and B spending, and also risk adjustments. Can you talk a little about what that would mean in practical terms for hospitals with this cost target?
LM: Yes. The specifics on how CMS gets to that, I’m not an expert on it, but I do understand it to be the hospital data, like a trailing three years prior to that DRG. If a hospital has CABG procedures, they’re going to look at that historical data to come to the target price. There’s some regionality to it because a hospital in one location in the US, let’s say Florida, versus New York or Iowa, would be different. So there are different aspects to how CMS determines that targeted price, and then there is some risk adjustment as well. But basically, it is built on three years of baseline data, it’s trended forward, and it’s set by DRG and at the regional level. That’s the basic premise. There are some other nuances, Natalie, to it, but that’s the basic premise. So, a hospital certainly can get its arms around the CMS TEAM payment model. They’ll probably already have their data, or they’re getting it maybe in a month, but that’s why it’s so important for hospitals to get their own data so they have a baseline.
First, it’s a five-year bundled payment. So it’s five years. First year is really the year where CMS is saying we’re going to just allow you to have upside, right? There’s no downside risk. This is the year where hospitals really can—they call it a glide path—where they can really understand what their costs are and still strive to get bonus payments back. This is a really phenomenal year for hospitals to make some money, to quickly put a plan together. The plan’s not going to be perfect, but it’s plan, adjust, plan, adjust. But really, if they can do these things now and get ahead of the curve, they can make money and then have a lot of learning for year two, where there is upside, downside.
So the key point is really understanding the true costs of care for a patient, let’s say for CABG or for a knee replacement, understanding their true cost, and that’s primarily a lot of it is the post-op, the post-surgery, those thirty days. How do we keep patients safe, optimized, and not being readmitted, and in the right placement? Does a patient need to go to an SNF versus home, and what does that look like? How are we managing that process?
Levers Hospitals Can Pull to Stay Below Target Costs
NF: Okay. And are there specific things that hospitals can sort of… levers they can pull that will help keep them underneath the target cost, but still providing quality care?
LM: Yes. I mean, I think there are a couple of levers for the CMS TEAM payment model. I’m going to talk a little bit about the post-op side because I know that’s of interest, but I’m also going to eventually move to what they can be doing in the hospital.
- Shifting patients to lower-cost post-acute settings when appropriate
- Strengthening partnerships with SNFs and rehab providers
- Reducing readmissions, a major cost driver
- Shortening length of stay in skilled nursing facilities
- Moving eligible cases to outpatient settings
- Understanding the true surgical cost, which is often overlooked but critical
A lot of hospitals are focused on the post-op side, which they should be; they’re big drivers of cost, but I feel there needs to be a real understanding of what’s being utilized in surgery, and those—all five cases are surgical.
Why Real-Time Surgical Data Matters in CMS TEAM Payment Model
NF: Yeah. And that segues really nicely into my next question, which is, let’s get into that surgical situation and understanding the true cost in an operating room or procedural room. Let’s talk about the importance of data. What do hospitals need to know? And why is accurate real-time data so important for the CMS TEAM payment model?
LM: If you think about it, data from any perspective is important. Data—you look at a patient coming into a hospital and being like doing the scheduling and understanding, let’s say, any of those issues why the patient’s not getting their pre-op testing done. Well, that’s an important data point. We talk about once a patient is discharged and wherever they’re going—whether it’s home or a rehab facility or what that looks like—that data point is important. The health of the patient—so heavier patients, or if they have co-morbidities—all those data points are important. So data is really important in terms of how we care for patients. Likewise, in the surgical environment, data is really important.
And so if you think about what supply items and implants are used in surgery, statistics show that only 48% of those items that are used in surgery are captured. So now you’ve got 50% of those items, supplies, or implants, not captured. Yes, some of them are captured outside the surgical environment in a paper way, or running things down post-case? Yes, some of that is—in our experience, Natalie—a lot of it isn’t. And so what happens is that hospitals are doing some sort of reworking. So they’re putting miscellaneous items, or maybe they’re just quickly saying, “Okay, it’s this catheter. It’s similar. I’m good. I’ve got to tend to the patient, which is important, right? I’m just documenting. I got to get back to supporting the surgical environment.” So if a hospital is only collecting in real-time and even post-case, possibly add another 10%. So we’re thinking 50 to 60% accuracy at best, capturing all of the supply and implants. How can they understand the true cost, particularly in these five cases, which are so high-cost?
This is a big concern for me, where hospitals are saying, “Oh, well, I have this one episode payment.” For example, we’re getting $52,000 for a CABG and maybe $30,000 or $20,000 or whatever that may be, post-op care, all the services. If they don’t understand that inpatient hospital costs are $30,000 or whatever that may be, then the analysis won’t be correct. So we’ve got to make sure that everything is understood in real time in surgery at the point of use.
How IDENTI Medical Snap&Go Supports TEAM Success
NF: And one tool that is an asset to hospitals to really capture real-time product and implant usage is IDENTI Medical Snap&Go. It’s designed to really give hospitals full visibility with real-time data collection using computer vision and machine learning. Can you talk a little bit more about what advantage that real-time data capture gives hospitals for the CMS TEAM payment model?
LM: Right, so I’m going to move back to the current state. The current state is a lot of manual entries, right? The current state is a barcode. Barcode is—I don’t know the exact percentage—but maybe, I think it’s something like 30 or 40% accurate, and the accuracy is because it is an older technology. Even though it is used, a lot of times those items aren’t being picked up. Then, if you go into systems, sometimes not all the data is in the system. So we can’t—even if the barcode’s working, if the data is not in the system and the barcode, he can’t find it, there are multiple barcodes on an implant box or supply box. So there are all these problems. The current state is incredibly problematic.
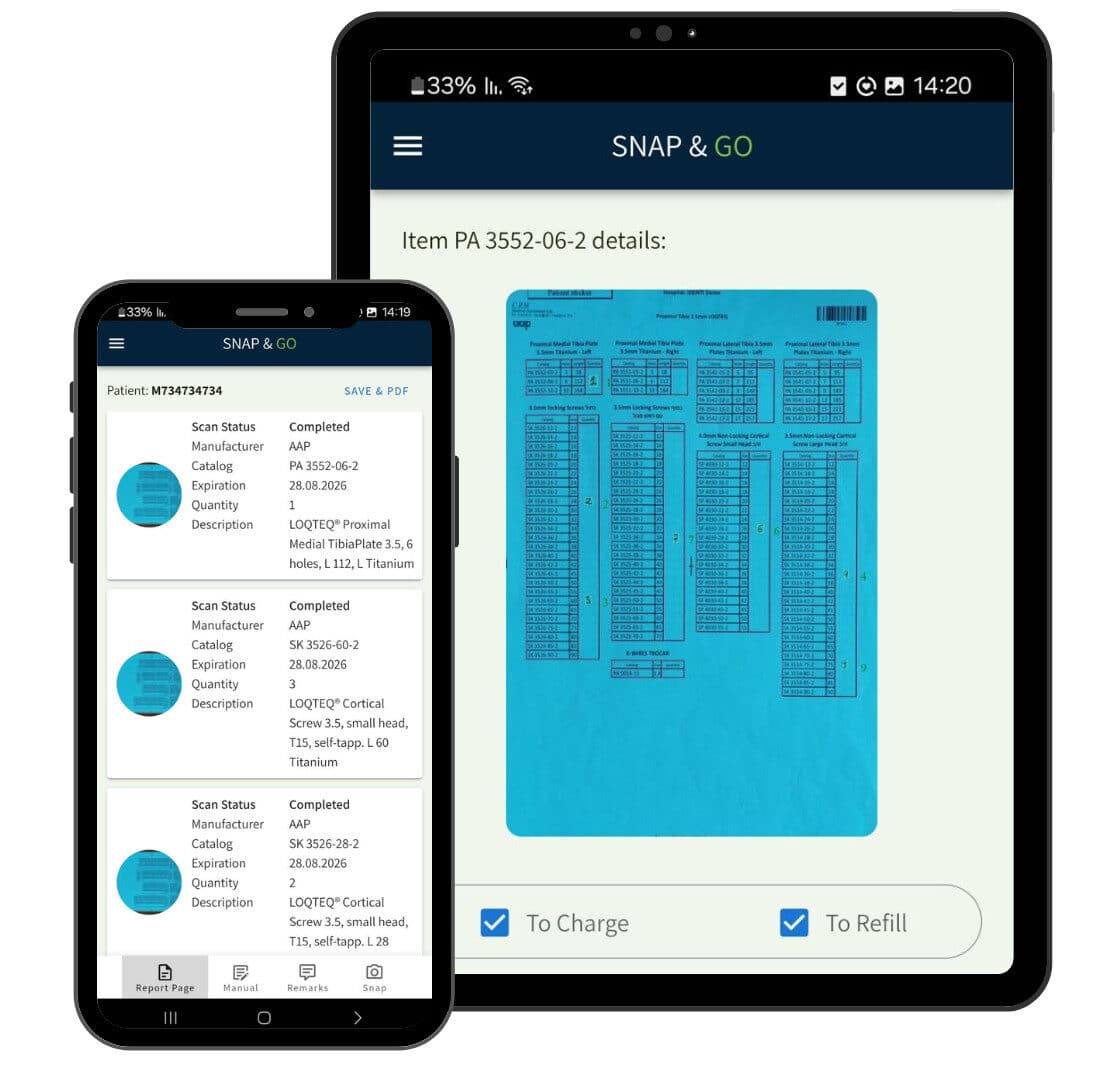
I often talk to CFOs and other finance leaders, and I think they’re surprised to understand, like, “Oh, we have technology,” and it’s like, “Well, barcode technology is old technology,” and a lot of hospitals are doing things manually. In the Cath lab, there’s a lot of manual input. That’s the current state, and now you move to AI-driven camera technology from IDENTI, which is so revolutionary.
If you think about it, it is brilliant. Camera technology is used globally. It can capture 100% of all the products used in surgery in real time and quicker than going through a barcode or manual entry because it’s literally putting an item under a camera. So that camera takes the full picture of everything on the box or package, and when all that data is taken from camera technology, IDENTI Medical’s AI system reads that and then integrates it seamlessly, literally in seconds, into the hospital’s system. What that means is that in real time during surgery, a hospital can capture 100% of supplies and data, and I think that is absolutely extraordinary. It’s going to mean immediate revenue impact for hospitals.
So that lift in revenue is because you’re capturing everything. Outside of Medicare, you’re going to be able to bill in other situations, but in this CMS TEAM payment model, we’re going to be able to identify what the true cost is, what the understanding of what is really being used.
And second, there are some exclusions for new technology. There are some specifics so that new technology—where there are new implants or new items—typically are not in a hospital’s system. If you’re using something new now, you’ve got to make sure that’s manual entry. Now you would get an extra payment for that, and those are the areas that we see as the biggest problem. So anything new comes in a surgical suite, in a procedure, those new items go under Snap&Go and computer vision technology captures it automatically, and there’s nothing post-op that has to be done.
What Should Hospitals Do Today to Prepare for TEAM?
NF: Yeah, it really shows you that, like you said, the true cost of what a surgery is. And with the integration into hospital systems, I feel like that also supports the workflow that needs to happen as the patient goes beyond just the surgery room. You can utilize the data for the thirty days post-op as well. All of it’s electronic and easily integrated. So thank you so much. I wanted to follow up just with one last question and ask if a hospital could do one thing today, two months out to prepare for the CMS TEAM payment model, what would it be?
LM: Yeah, I think if I were in a hospital and I were doing the one thing—I think there are many things to be done—but if there’s one thing I would want to understand the data in every single instance, the full journey—the journey of the data.
I’d want to understand it pre-op, understand my patient mix by DRG, understand where I might need to—the hospital might need to—add interventions because different hospitals have different communities, so the interventions are going to be different.
Post-op, same thing in the hospital environment, that surgical environment—I think it’s unequivocally so important for hospitals to really understand what implant supplies are being used, particularly because we want to share that with the surgeons. The surgeons are scientists; you give them the data, and they have to trust the data. They will trust data from camera technology. They’re using high-tech digital cameras, all kinds of technology, robotics, and now we’re going to bring that into the business side of healthcare. They’re going to trust it. So this is so key. I would want to get data all across the thirty days, particularly in the surgical environment, present it to physicians, and start having those discussions like, “There are some variations in what’s being used; how do we collaborate together?”






