What’s inside:
- How a single missed surgical charge capture event triggers delays, denials, and costly workflow disruptions
- A detailed breakdown of the domino effect across clinical, supply chain, and revenue cycle teams
- The financial, operational, and compliance risks associated with incomplete surgical documentation
- Why EHRs and barcode systems alone cannot eliminate missed surgical charge capture
- Strategies hospitals can use to protect revenue, reduce administrative burden, and improve OR documentation accuracy
Across hospitals of every size, one operational issue consistently undermines financial stability and workflow accuracy: missed surgical charge capture. Even a single undocumented implant, tray, or supply item costly chain reaction; pulling clinical teams away from patient care, derailing supply chain processes, slowing revenue cycle throughput, and weakening compliance readiness.
As hospitals search for ways to strengthen OR workflows, control labor costs, protect margin, and improve operational performance, the real question becomes: “How do missed charges ripple across the organization, and what is the actual cost of this disruption?” This white paper reveals how one documentation gap creates enterprise-wide inefficiencies that drain resources and erode financial performance.
Why Does Missed Surgical Charge Capture Occur in the OR?
The Realities of Surgical Workflow
The OR environment is inherently incompatible with manual documentation. High-pressure, fast-paced intraoperative workflows create predictable opportunities for missed charges due to:
- Rapid, unplanned procedural changes
- Unexpected product usage
- Rotating and multitasking staff
- Failed barcode scans
- Time-sensitive decisions that interrupt documentation
These challenges persist even with digital tools because EHRs and scanners still require manual human action at moments when clinical focus is appropriately on the patient, not documentation.
Why Scanning and EHR Tools Don’t Solve the Problem
Leaders often ask why missed charges continue despite EMRs, digital preference cards, and barcode systems. The reason is simple:
Manual documentation workflows do not align with real surgical conditions.
Legacy workflows, with barcodes or manual key-in entries, require staff to pause and intervene at the exact moment supplies are used, a process that does not align with high-pressure surgical conditions. These limitations are especially problematic in implant-heavy specialties, where preventing missed surgical charge capture is critical for accurate billing and reimbursement.
To break this pattern, hospitals need technology that captures product usage automatically in the background, without disrupting intraoperative workflow.
IDENTI Medical’s AI camera technology captures supply and implant usage instantly and accurately, reducing manual follow-up, improving documentation reliability, and supporting stronger coordination between clinical and administrative teams. With Snap&Go, hospitals capture 100% of surgical supply usage in real time, eliminating the operational and financial strain caused by documentation gaps. IDENTI Medical’s computer vision can capture more product usage and data than manual EHR- or scanner-based workflows, helping hospitals protect staff time and reduce the downstream impact of missed charge capture.
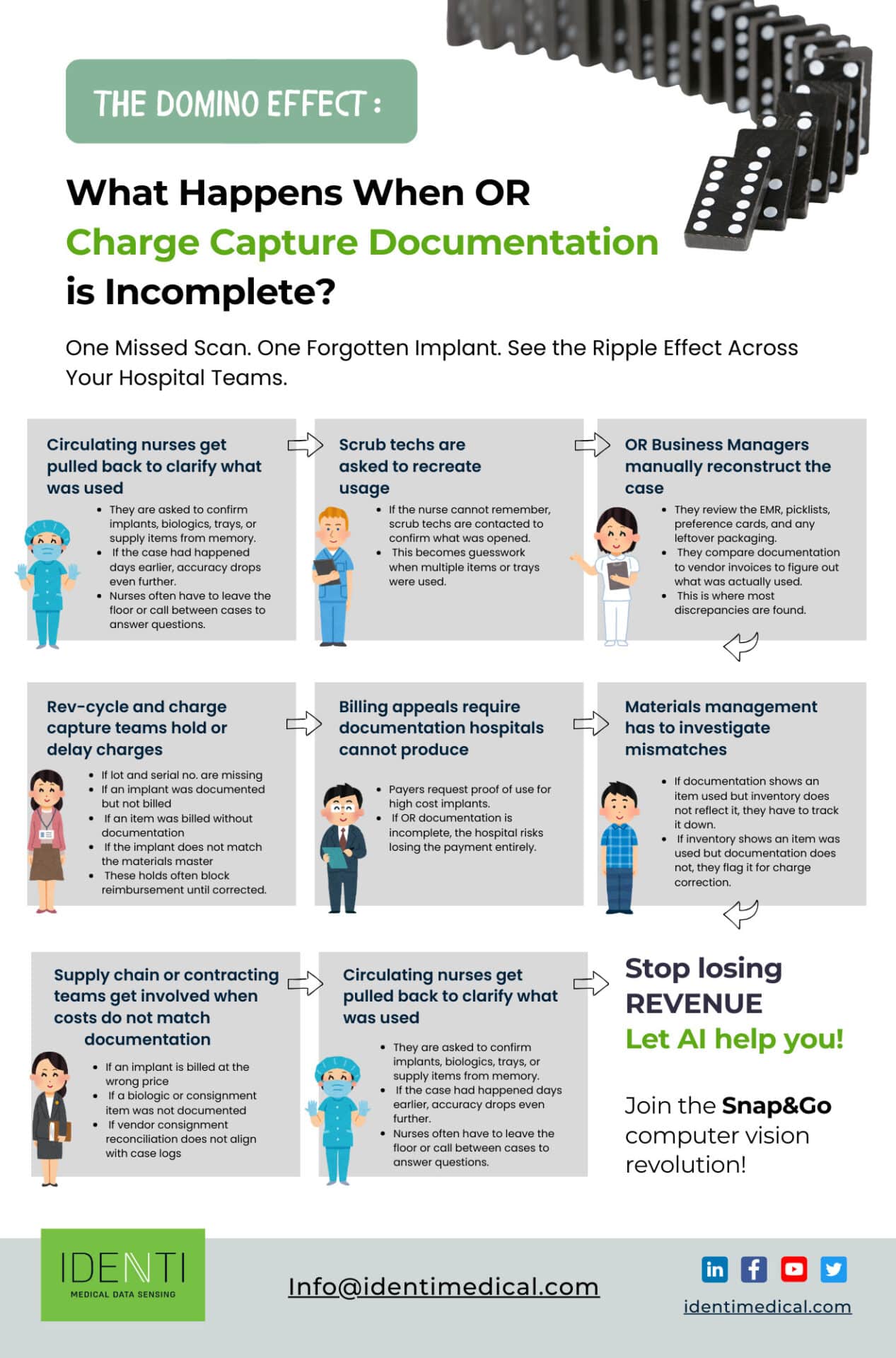
The Domino Effect: How One Missed Surgical Charge Capture Becomes a System-Wide Problem
What’s at Stake: A single missed charge doesn’t stay isolated; it becomes the starting point for labor waste, revenue leakage, and system-wide workflow breakdowns.
Step 1: Clinical Staff Pulled Back Into Recollection
Circulating nurses and scrub techs are interrupted post-case to reconstruct usage from memory.
This rework consumes clinical labor, distracts staff from patient care, and introduces uncertainty into documentation.
Step 2: OR Managers Begin a Forensic Rebuild
If clinical recall is incomplete, OR managers must rebuild the case using:
- EHR case notes
- Preference cards
- Picklists
- Packaging remnants
- Vendor usage confirmations
This time-consuming process exists almost exclusively because of missed surgical charge capture and diverts managers from strategic work.
Step 3: Revenue Cycle Teams Face Delays and Denials
Revenue cycle leaders frequently research how missed surgical charge capture leads to payer denials and delayed reimbursement. Incomplete documentation produces:
- Missing lot codes and serial numbers
- Unverified implant usage
- Claims placed on hold
- Record requests hospitals cannot answer
- Denials that require lengthy appeals
Every missed charge slows cash flow and inflates the cost-to-collect. And these issues compound quickly in high-volume surgical programs.
Step 4: Materials Management Must Resolve Inventory Conflicts
When system records and physical inventory don’t match, materials staff must determine:
- Products showing in stock when they were actually not
- Implants appearing “used” without documentation
- Discrepancies between OR logs and inventory counts
This not only consumes labor but risks stockouts, over-ordering, and financial write-offs.
Step 5: Supply Chain and Contracting Must Reconcile Vendor Data
Vendor bills often conflict with internal data when missed surgical charge capture occurs. Supply chain and contracting teams must manually reconcile:
- Invoice mismatches
- Consignment usage
- Pricing discrepancies
- Unverified biologics
This labor adds hidden cost and delays financial reconciliation across the organization.
Financial Impact: What is the True Cost of Missed Surgical Charge Capture?
Revenue Leakage Adds Up Quickly
Hospitals frequently research questions such as:
- “What is the cost of incomplete surgical charge capture?”
- “How much revenue is lost from missing implant documentation?”
The financial implications are substantial. Missed surgical charge capture contributes to:
- Underbilling for implants and biologics
- Claim denials due to missing proof-of-use
- Unrecovered costs for high-value devices
- Inaccurate service line profitability analysis
In implant-dependent specialties, even minor documentation gaps create significant revenue leakage.
Delayed Cash Flow and Increased Denials
Payers require precise proof-of-use for costly devices. Missed surgical charge capture commonly leads to:
- Increased accounts receivable days
- Audit challenges
- Medical necessity denials
- Reimbursement delays
These interruptions weaken the financial performance of entire perioperative programs.
Operational Impact: How does it Impact Workflows and Labor Costs
Staff Time Consumed by Backtracking
Every incident of missed surgical charge capture demands workarounds that erode operational efficiency. Nurses, scrub techs, OR managers, materials staff, and revenue cycle teams collectively lose hours to reconstructing surgical documentation accuracy.
Hospitals often underestimate this labor burden until they begin tracking how much staff time is lost due to missed surgical charge capture documentation.
This cycle erodes operational efficiency and adds stress to already overextended teams.
Workflow Disruptions and Burnout
Repeated reconstruction tasks create frustration, reduce productivity, and elevate stress. Over time, this contributes to burnout and increases staff turnover in perioperative roles.
Compliance and Patient Safety Concerns
Traceability and Recall Challenges
Compliance leaders must maintain accurate device histories, yet missed surgical charge capture results in gaps that affect:
- Implant tracking
- Lot and serial number documentation
- Biologic traceability
- FDA reporting
- Recall readiness
Hospitals often discover during audits that traceability gaps resulting from missed surgical charge capture create substantial regulatory risk.
Why do Charge Capture Issues Persist?
Even with EHRs and scanning systems, OR documentation remains dependent on manual human workflows. The OR’s dynamic environment makes consistent documentation difficult. The domino effect will continue until hospitals adopt processes and technologies that:
- Reduce reliance on manual scanning
- Capture real-time product usage
- Auto-populate required device identifiers
- Integrate OR, supply chain, and revenue cycle data
- Prevent documentation gaps during complex procedures
Many leaders now search for AI-powered point-of-use charge capture optimization solutions to reduce missed surgical charge capture in high-volume surgical departments, recognizing that manual processes cannot keep pace with modern surgical demands.
Breaking the Chain Reaction

Missed surgical charge capture is not a small clerical error; it is a systemic disruption affecting clinical accuracy, financial performance, supply chain integrity, and regulatory compliance. A single documentation gap can force clinical teams to reconstruct supply usage, burden OR managers with forensic tasks, complicate inventory reconciliation, and trigger revenue cycle delays.
Hospitals that proactively address missed surgical charge capture strengthen their entire perioperative ecosystem, reduce preventable revenue loss, and improve operational stability across departments.
Download the infographic here and contact us to schedule a Snap&Go demo today.






