What’s inside:
In this white paper, you’ll discover the 13 most common charge capture gaps costing U.S. hospitals millions each year, along with the compliance, operational, and financial risks they create.
Learn how outdated manual workflows lead to missed charges, vendor disputes, data errors, and audit failures, and how AI-powered automation like IDENTI’s Snap&Go transforms charge capture at the point of care. From revenue leakage to Joint Commission readiness, this paper breaks down what’s at stake and how hospitals can protect their margins with real-time, automated documentation.
Charge capture remains one of the most vulnerable points in a hospital’s revenue cycle. Industry estimates suggest hospitals lose 1–2% of net revenue annually to missed or incomplete charge capture. Despite the stakes, hospitals are still relying on outdated tracking methods: barcode restrictions, delayed manual entry, and siloed hospital systems. These manual systems not only delay reimbursement but also create blind spots that compromise financial, operational, and clinical performance.
That’s why hospitals are turning to real-time automation to modernize charge capture at the point of care. IDENTI Medical’s Snap&Go is one such solution: an AI-powered camera platform built on computer vision, machine learning, and real-time cloud integration. It automatically identifies, documents, and transmits item usage as it happens. By embedding intelligent automation directly into clinical workflows, Snap&Go replaces error-prone documentation with real-time, automated item tracking that enables near-complete charge capture and accurate, audit-ready data that strengthens financial performance and supports better decision-making across the organization.
This white paper analyzes 13 specific charge capture challenges that drive financial leakage, operational inefficiency, and compliance risk and explains how Snap&Go addresses them with AI-powered automation.
The Financial Impact of Missed or Delayed Charge Capture
Missed or delayed charges directly drain millions from the bottom line and threaten reimbursement under new CMS models.
1. Manual Case Corrections Delay Billing
Manual charge capture, validation, and correction is a routine bottleneck in the revenue cycle. After a surgical case, billing often waits on validation of the used implants and supplies. And delays cost you; studies show that up to 25% of charges are lost if entry occurs more than 72 hours post-procedure. The longer the lag, the higher the risk of forgotten items, inaccurate coding, and unbilled revenue.
2. Missed Charges That Go Undetected
Services rendered but not billed are among hospitals’ top financial threats. Causes include documentation errors, communication gaps, and inadequate charge capture processes. These breakdowns in the charge capture workflow lead to revenue loss that often goes undetected until audits or denials arise. In one survey, 72% of respondents identified missed charges as a top concern with their charge capture process.
3. Lost Carve-Out Reimbursement
Specialty implants and high-cost devices are often reimbursed separately through carve-outs in payer or vendor contracts. When these go uncaptured, payors can deny or reduce costs, and hospitals lose this revenue due to missing proof of use, incomplete data, or absent vendor sheets.
4. Preparing for CMS TEAM Bundles
In January 2026, CMS’s new payment structure, Transforming Episode Accountability Model (TEAM), will require hospitals to accurately document all episode-of-care costs in orthopedics, cardiac, and other service lines. Hospitals will receive a single, fixed bundle payment for an entire episode of care, meaning that hospitals must effectively and accurately manage documentation, and a missed or incorrect charge reduces the hospital’s opportunity to demonstrate accurate cost reporting and may lead to reduced reconciliation payments or penalties.
How Snap&Go helps:
- Captures 100% of items at point of use — including non-catalog or bill-only items
- Automatically syncs product data (UDI, lot, serial, expiry) into ERP/EHR for real-time billing
- Provides proof-of-use images for payer and vendor audits
- Enables faster bill drop and accelerates revenue recognition
- IDENTI’s back-office reviews missing data, ensuring charge completeness
Operational and Compliance Risks from Manual Workflows
Manual workflows increase operational costs, slow reimbursement, and expose hospitals to clinical and financial risk.
5. Bill-Only Items Tracked by Hand
Occasionally, surgeons don’t know exactly what item or size they will need for a patient until they are in the operating room. A vendor representative will bring a selection of items before the procedure for the surgeon to choose from. These bill-only items are not stocked or preloaded into the hospital system and are usually tracked manually after use. A real-world consequence: vendor reps fill out handwritten usage sheets after the procedure. These sheets are error-prone, frequently misplaced, and include important patient data that could put hospitals at risk when vendors walk out with them. This practice also poses a security risk, as handwritten logs may contain protected health information, which can raise compliance and audit concerns.
6. Vendor Disputes Over Consignment Stock
Consignment stock, items stored on site but only paid for when used, can lower a hospital’s upfront costs but requires accurate, timely usage tracking to reconcile with vendors. While some hospitals use automated inventory systems, many still rely on spreadsheets or manual logs, leaving room for mismatches. Discrepancies between hospital and vendor records can delay payment, trigger disputes, and lead to unexpected restocking fees. Without standardized, real-time documentation, reconciling consignment usage becomes labor-intensive and error-prone, impacting both vendor relationships and revenue integrity.
7. Expired Items Discovered Too Late
Managing expiry dates manually is error-prone and risky. A Cardinal Health survey found that 1 in 4 clinicians have seen or heard of expired items used in patient care. Beyond a compliance risk, expired products can jeopardize patient safety, increase liability exposure, and lead to regulatory penalties. They also complicate accurate charge capture, especially when post-procedure corrections are required to account for substitutions or discarded items.
How Snap&Go helps:
- Digitally tracks bill-only and consignment items, even if not preloaded in the system.
- Aligns vendor records automatically, reducing disputes and true-up cycles.
- Flags expiration issues in real time before use.
- Automates logging, reducing admin burden and risk.
Data Integrity Challenges That Disrupt Decision-Making
Incorrect or missing data undermines decision-making, inflates costs, and creates blind spots across finance, supply chain, and clinical teams.
8. Use of “Miscellaneous” Codes That Hide True Costs
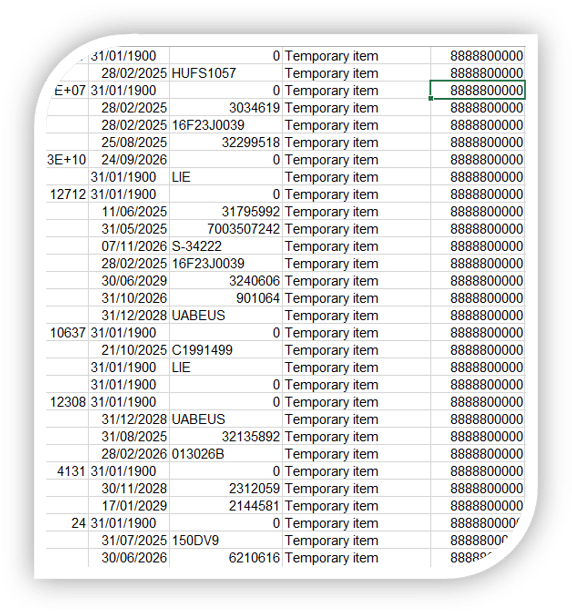
When items aren’t in the system or barcodes fail, hospitals will use catch-all, generic codes (e.g., 000000). While this is intended as a stopgap, these items corrupt the item master, creating confusion and inefficiencies, and the scale of its impact is often underestimated. This skews service line reporting, hides costs, and disrupts profitability tracking by procedure.
9. Weak Data for Payer Negotiations
Without standardized usage data, hospitals have a hard time justifying reimbursement rates for complex procedures or new technologies. For example, if a payer challenges the necessity of a high-cost biologic implant, but the hospital can’t immediately produce standardized data showing frequency, patient need, and outcomes, the negotiation often ends with lower reimbursement or denial of coverage.
10. Unreliable Physician and Service Line Profitability Analysis
Hospitals increasingly rely on service line analysis to align cost, revenue, and quality. But when data is scattered across EHRs, spreadsheets, and inventory systems, fragmented records prevent hospitals from accurately tracking charge capture and cost variation by surgeon or case type. It is nearly impossible to produce a clear report, and poor data erodes physician trust and impairs service line development.
11. Misalignment Between Item Master and CDM
The item master tracks inventory; the CDM governs billing. When these systems don’t align, hospitals risk underbilling, missed charges, and compliance issues. Vizient found that over 30% of item master data contains errors—such as outdated pricing, duplicates, or incorrect descriptions—which can prevent items from being billed correctly. When items aren’t mapped to the CDM, staff often rely on “miscellaneous” codes, distorting financial data and making accurate reporting and reimbursement more difficult.
How Snap&Go helps:
- Captures complete, standardized item data (manufacturer, catalog number, lot, expiration) at the point of use
- Feeds ERP and EHR systems with validated usage data in real time
- Reduces reliance on “miscellaneous” coding
- Enhances item master and CDM alignment via enriched data upstream
- Supports accurate, granular reporting for finance and clinical leaders
Compliance, Accreditation, and Staff Burden
Manual charge capture increases audit risk, hurts staff morale, and diverts attention from patient care.
12. Joint Commission Audit Vulnerability
Accreditation can happen anytime. A Joint Commission audit can significantly impact a healthcare organization’s revenue cycle by influencing reimbursement rates, network participation, and overall financial performance. Incomplete or inaccurate documentation can lead to failed audits, denied claims, and increased compliance costs. A robust charge capture framework ensures that required documentation is complete and verifiable at every stage of care delivery.
13. Documentation Burden on Nurses
Manual product logging adds to a clinician’s workload. Nurses find themselves applying stickers, recording product details, or validating usage sheets; meaning steps that are the foundation for a healthy revenue cycle are their responsibility, while also focusing on patient care. AORN found that the burden of administrative documentation contributes to burnout, increased errors, and a decrease in job satisfaction.
How Snap&Go helps:
- Creates traceable, standardized proof-of-use records, so documentation is always complete and audit-ready
- Stores vendor documents and Instructions for Use in a digital format
- Frees nurses from manual entry, improving satisfaction and care quality
Modernizing Charge Capture With AI Automation

In today’s value-based landscape, charge capture must evolve from a fragmented, manual afterthought into a strategic pillar of revenue integrity and a reliable, real-time source of clinical and financial truth. Snap&Go provides hospitals with a future-ready foundation: automating charge capture at the point of use, enriching data upstream, and integrating seamlessly with core systems. The result is more than accurate billing; it’s accelerated reimbursement, audit-proof compliance, and actionable insight that empowers leaders across finance, supply chain, and clinical operations.
As regulatory models like TEAM demand complete cost transparency and tighter accountability, hospitals that invest in intelligent automation today will be the ones best equipped to lead tomorrow.
Contact us to learn how Snap&Go can revolutionize your charge capture process.






